What Is The CA-125 Test And Why It Matters
Most people know the usual health checks – blood pressure, cholesterol, maybe sugar. All are useful, but they don’t tell everything. Some conditions don’t appear on those. That’s where markers like CA-125 step in. It’s a protein circulating in the blood. For some, levels remain low. For others, it rises, and doctors watch closely because it can connect with ovarian cancer and possible other problems.
The test itself is called the CA-125 blood test. It is easy to do. It’s just a tube of blood, a quick draw from your arm, nothing stressful for the patient. But behind that small sample there is a big revelation. The result might guide doctors examining more closely, or reassure that things look stable.
At Longevity Clinics, we keep tools like this in our set because prevention isn’t about waiting. It’s about looking where issues might hide, and catching them before they settle in. CA-125 isn’t perfect, no test is, but used the right way it’s another step in long-term health planning.
CA-125 falls within the category of tumour markers, which are things that occasionally go up in the presence of cancer. Epithelial ovarian cancer is the most closely related to this case. Doctors rely on it when coming to a certain diagnosis, determining how the treatment is working or later, seeing whether cancer has come back.
But here’s the messy part. Numbers go up for other reasons too — a regular menstrual cycle, endometriosis, pelvic infections, even pregnancy. So a higher reading does not equal ‘you have cancer’. And a normal reading doesn’t always mean you’re clear. That’s why the test shows a bigger picture.
At our clinic we don’t share numbers without context. We line them up with history, symptoms, other lab results, maybe imaging if needed. That’s how it makes sense.
Think of it like a signal light — not a diagnosis by itself. Levels tend to climb in women with certain ovarian cancers, but also in other cases. Doctors use it in three ways, mostly to:
It’s especially relevant for women over 40 and anyone carrying genetic risk like BRCA1 or BRCA2 mutations. For them, this marker can be part of regular check-ups.
And while the headline is cancer, the wider story is precaution. A test like this needs to have a closer look. If the reading is fine, that’s great. If it’s off, then more checks are triggered sooner. Either way, it shapes decisions about what comes next.
From the outside it’s simple. Sit down, sleeve up, a nurse cleans the skin, puts in a small needle, draws a vial of blood. That’s it. No fasting and no special prep is needed. There may be a sting, and may be a bruise later, usually nothing more.
The lab runs the sample. Numbers come back in units per millilitre (U/mL). Under 35 is often called normal, though labs may vary. Numbers above that need looking at.
At Longevity Clinics, once results arrive we don’t just pass them along. We sit down, explain what the number might mean, and how it ties into your story. For some, it means rechecking later. For others, it can mean extra scans or tests. The value is not in the vial of blood, it’s in how the result is used.
Ovarian cancer is difficult because it hides early. Symptoms like bloating, feeling full quickly, and vague discomfort overlap with everyday issues. That’s why it’s called the silent one. By the time it’s obvious, the disease is often advanced.
The CA-125 test can be used to open the window at an earlier time. Doctors receive a baseline before the treatment process begins. Then they test again as chemotherapy or surgery advances. Declines and decreases indicate treatment is effective. An increase in numbers can be an indicator of trouble.
It isn’t foolproof. Sometimes women with ovarian cancer don’t show high CA-125. Some women without cancer do. But when used for the right patient, it’s a valuable piece of the process.
Our role is helping people understand this balance. The number by itself is not a sentence. It’s a clue.
Most of our patients aren’t here just for today. They want the years ahead to be healthier. The CA-125 test fits that — not because it’s the only answer, but because it adds another layer of insight.
For women with family history, or genetic risk, or unexplained symptoms, this test gives direction. It’s proactive, not reactive. And that’s the mindset at Longevity Clinics: act early, don’t wait for things to grow.
CA-125 is one marker, but health isn’t about a single number. For ovarian cancer especially, early detection changes everything. Survival and treatment options improve if the disease is found before it spreads.
That’s why doctors often pair CA-125 with imaging like ultrasound or MRI. It isn’t used to screen everyone, but targeted where risk is higher.
We also view it as something that falls into a bigger picture at Longevity Clinics. In conjunction with CA-125 we monitor other markers, hormones, and cholesterol, to see if there is inflammation. We also, at times, include genetic panels. Collectively they create more than a snapshot. They create a profile and a map of health direction to come.
And this goes on to map the wider risks. The five most prevalent risks which play a role in health outcomes are cancer, heart conditions, metabolic, neurodegenerative diseases, and skeletal weakness. Analysing these risks can lead to prevention.
Patients often want the details about what happens exactly. It goes like this:
The entire procedure is simple and fast, taking under ten minutes. But what matters is what follows. At Longevity Clinics, results aren’t just emailed with a number. They’re explained. Numbers are tied to context, history, family, and lifestyle. That’s where meaning comes in.
The common cut-off is 35 U/mL. Below that figure is usually normal. Above, it might mean ovarian cancer, but it might also mean endometriosis, menstruation, infection, or another benign cause.
So interpretation is everything. Doctors will ask:
From there, the path may be to watch and repeat later, or order extra scans. No single number is ever the answer.
This is where we spend time with patients, not just telling them the figure, but unpacking it and making sure they understand it’s one piece, not the whole story.
In the event that a person already has ovarian cancer, the CA-125 test has an alternative role to play — not by guessing, but by keeping track. Treatment will not begin until doctors have checked the numbers. That’s the baseline. Then, every two or three weeks or months, new tests are done. Usually, by the downward numbers, it means the treatment is effective. The CA-125 to follow should be in case chemotherapy or surgery is shrinking the cancer.
In case numbers begin to increase again, it may be a good indicator that the disease is reoccurring. Or at other times the patient is okay, with no symptoms but the marker is different. This is why specialists maintain surveillance during treatment with frequent examinations, to check when symptoms begin to emerge.
But it doesn’t work perfectly for everyone. Some cancers don’t produce much CA-125 at all. In those cases, relying on the marker would give false confidence. That’s why doctors mix it with imaging, ultrasounds, MRIs, and CT scans. At Longevity Clinics, we keep it in context with a combination of tests, never just the marker on its own.
Every check looks the same: a vial of blood, a lab report. But the meaning changes depending on timing.
Patients often ask how often they’ll need it. The answer depends. Some may need it every month, some every three months. It’s tailored. What we do is walk patients through it, so the test doesn’t feel abstract. They see how it connects to the bigger plan.
A normal level doesn’t always mean safe. A high level doesn’t always mean cancer. That’s the challenge.
In one case, such as during menstruation, CA-125 may shoot. The same may happen due to endometriosis or pelvic inflammatory disease, and even in some liver diseases.
Flip side: some women with ovarian cancer show completely normal CA-125. That’s the false negative. It is dangerous if the marker is the only check. That’s why at Longevity Clinics we always stress: the test is part of the toolkit, not the whole thing.
When levels change, we look deeper. We may order a transvaginal ultrasound, maybe a CT or sometimes a biopsy. The blood result is the nudge, not the verdict.
CA-125 is not a screening test for everyone. That’s important. The National Cancer Institute in the US doesn’t recommend it as routine screening for women without symptoms or risk. Too many false positives can lead to stress, unnecessary scans, and invasive biopsies.
The dangers are not so large but they are present. A biopsy, for example, has a risk of infection, bleeding, and tissue destruction. There can also be an emotional cost. Weeks of anxiety await the victim of a false alarm. We do not take the test casually. It is applied where it makes sense, for high risk patients, treatment monitoring, and symptom investigation.
At Longevity Clinics we explain this upfront. It is better to know the limits than think it’s a magic bullet.
It’s not for everyone. But for some, it’s worth asking about if they are:
In these groups the test can guide decisions. Outside of them, it’s less clear. That’s why a conversation with a healthcare provider matters more than the number alone.
Prevention is the key to longevity. The longevity of life is not just due to diet and exercise. It is the process of solving issues before they escalate into a crisis.
CA-125 fits here. It does not substitute mammograms or colonoscopies or heart tests. But with the right patient it provides a way to act earlier.
At Longevity Clinics we don’t run it as a stand-alone service. It’s woven into a bigger package of biomarker testing. We analyse over a hundred markers, from inflammation to hormones, cardiovascular health, and metabolic risk. Together they give a map of where health is going. CA-125 is one tile in the mosaic.
Most people worry about the big five:
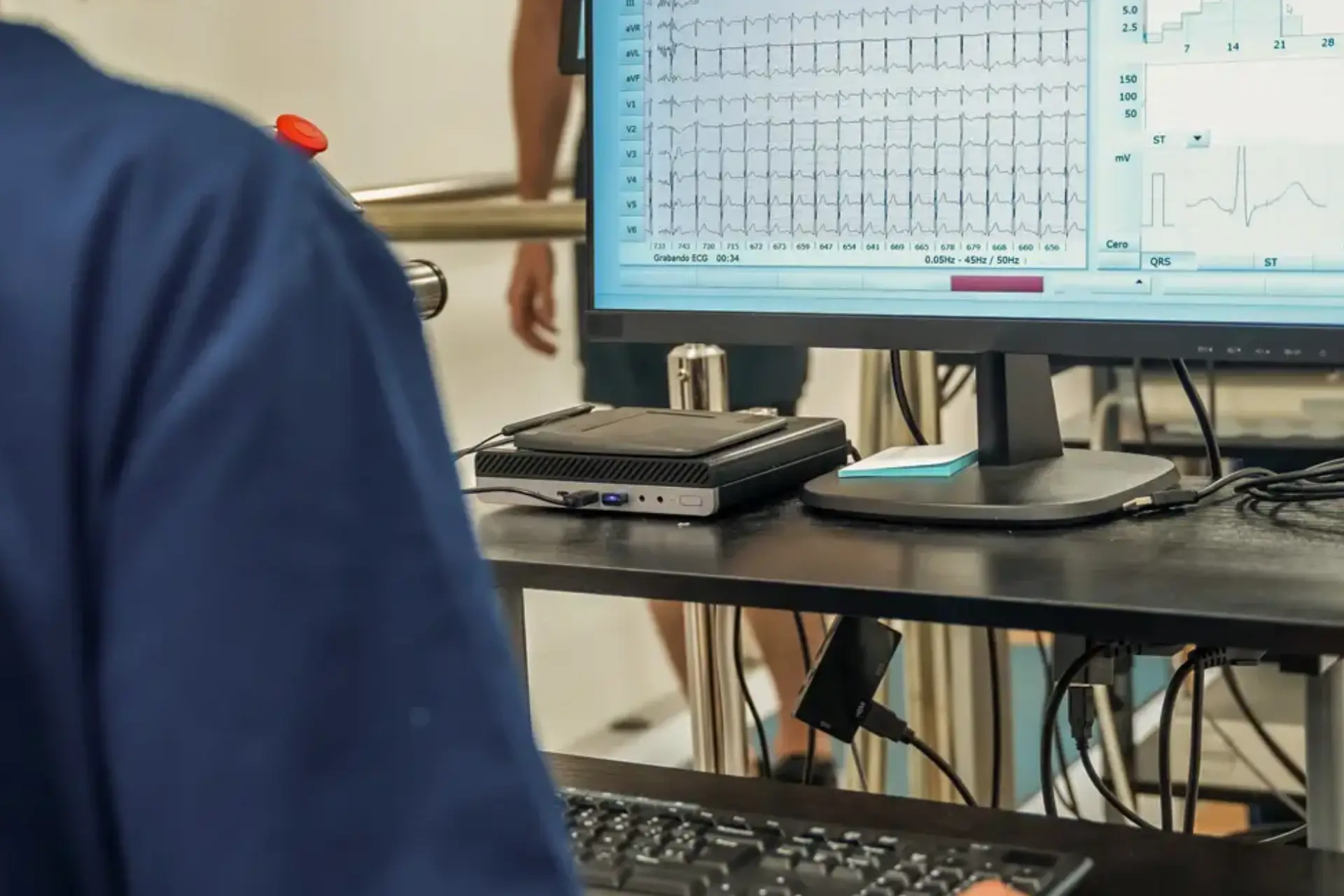
CA-125 speaks mostly to the first worry on the list. But we check others too — ECG of heart rhythm, DEXA bone density, MRI whole-body scan, microbiome analysis of gut health. Only alone are the tests helpful, but the combination of the tests relates to a narrative of risk and resilience.
So when a patient comes in asking about CA-125, we also ask: what else do we need to check? That way the focus isn’t too narrow.
Patients often describe the CA-125 test as easy. The hardest part is waiting for results. The test is nothing — five minutes, a mild sting, sometimes a small bruise, and no fasting or prep.
After, the waiting begins. That is why we strive to achieve speed and clarity in consultations with Longevity Clinics. Numbers might appear frightening if they are dropped on people without any context. We ensure there is a conversation along with the result and not just a figure.
For someone in treatment, the CA-125 becomes almost like a scoreboard.
It’s not perfect. Sometimes numbers rise briefly and then drop. Sometimes they stay stable while imaging shows change. That’s why oncologists never rely on one test. But as part of the pattern, it’s vital.
We explain this to patients so they don’t panic at every fluctuation. Context matters. Trends over time matter more than one number.
We don’t push CA-125 on everyone. We fit it to risk. When it’s used, it’s surrounded by other diagnostics. And when results arrive, we explain, we connect it to lifestyle, and to long-term planning.
Longevity Clinics is not about checklists. We put patients in charge of taking earlier action. CA-125 aids us in doing that.
We expand into longer conversations about healthspan as well, such as how blood analysis may be an incentive. Also, risk perception may increase adherence to nutrition, exercise, and stress management in a patient.
If results are normal, keep up monitoring and combine with other checks. If results are high, look deeper. Maybe look at imaging, or maybe another round of tests. If cancer is confirmed, the test becomes a tracker for treatment response.
Every path is different. That’s why personalised care is central. Numbers are universal, but what they mean is individual.
We guide patients through this path. We don’t just deliver results. We stay with patients for the decisions that follow.

We’ve developed a comprehensive six-step process that acts as your personal health roadmap, to follow towards your health goals.





